Animal Husbandry and Feed Science ›› 2023, Vol. 44 ›› Issue (4): 29-40.doi: 10.12160/j.issn.1672-5190.2023.04.005
• Basic Research • Previous Articles Next Articles
Research Progress in Molecular Regulatory Mechanisms in the Development of Non-alcoholic Fatty Liver Disease and Its Transition to Liver Cancer
BIAN Kangkun,BAO Yulong,WANG Li
- College of Basic Medicine,Inner Mongolia Medical University,Hohhot 010110,China
-
Received:2023-05-19Online:2023-07-30Published:2023-08-30
CLC Number:
Cite this article
BIAN Kangkun, BAO Yulong, WANG Li. Research Progress in Molecular Regulatory Mechanisms in the Development of Non-alcoholic Fatty Liver Disease and Its Transition to Liver Cancer[J]. Animal Husbandry and Feed Science, 2023, 44(4): 29-40.
share this article
| [1] |
BEGRICHE K, MASSART J, ROBIN M A, et al. Mitochondrial adaptations and dysfunctions in nonalcoholic fatty liver disease[J]. Hepatology, 2013, 58(4):1497-1507.
doi: 10.1002/hep.26226 pmid: 23299992 |
| [2] |
DIEHL A M, DAY C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis[J]. The New England Journal of Medicine, 2017, 377(21):2063-2072.
doi: 10.1056/NEJMra1503519 pmid: 29166236 |
| [3] | BYRNE C D, TARGHER G. NAFLD:A multisystem disease[J]. Journal of Hepatology, 2015, 62(Suppl 1):47-64. |
| [4] |
POCHA C, KOLLY P, DUFOUR J F. Nonalcoholic fatty liver disease-related hepatocellular carcinoma:A problem of growing magnitude[J]. Seminars in Liver Disease, 2015, 35(3):304-317.
doi: 10.1055/s-00000069 |
| [5] |
SERVIDDIO G, BELLANTI F, VENDEMIALE G. Free radical biology for medicine:Learning from nonalcoholic fatty liver disease[J]. Free Radical Biology and Medicine, 2013, 65:952-968.
doi: 10.1016/j.freeradbiomed.2013.08.174 |
| [6] |
COBBINA E, AKHLAGHI F. Non-alcoholic fatty liver disease (NAFLD) - Pathogenesis, classification, and effect on drug metabolizing enzymes and transporters[J]. Drug Metabolism Reviews, 2017, 49(2):197-211.
doi: 10.1080/03602532.2017.1293683 pmid: 28303724 |
| [7] |
FRIEDMAN S L, NEUSCHWANDER-TETRI B A, RINELLA M, et al. Mechanisms of NAFLD development and therapeutic strategies[J]. Nature Medicine, 2018, 24(7):908-922.
doi: 10.1038/s41591-018-0104-9 pmid: 29967350 |
| [8] |
KLEINER D E, MAKHLOUF H R. Histology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in adults and children[J]. Clinics in Liver Disease, 2016, 20(2):293-312.
doi: 10.1016/j.cld.2015.10.011 pmid: 27063270 |
| [9] |
SUMIDA Y, YONEDA M. Current and future pharmacological therapies for NAFLD/NASH[J]. Journal of Gastroenterology, 2018, 53(3):362-376.
doi: 10.1007/s00535-017-1415-1 pmid: 29247356 |
| [10] |
GOLDBERG D, DITAH I C, SAEIAN K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation[J]. Gastroenterology, 2017, 152(5):1090-1099.
doi: S0016-5085(17)30014-8 pmid: 28088461 |
| [11] |
LINDENMEYER C C, MCCULLOUGH A J. The natural history of nonalcoholic fatty liver disease-An evolving view[J]. Clinics in Liver Disease, 2018, 22(1):11-21.
doi: S1089-3261(17)30064-8 pmid: 29128051 |
| [12] |
PEJNOVIC N, JEFTIC I, JOVICIC N, et al. Galectin-3 and IL-33/ST2 axis roles and interplay in diet-induced steatohepatitis[J]. World Journal of Gastroenterology, 2016, 22(44):9706-9717.
pmid: 27956794 |
| [13] |
LIANG Z X, LI T A, JIANG S A, et al. AMPK:A novel target for treating hepatic fibrosis[J]. Oncotarget, 2017, 8(37):62780-62792.
doi: 10.18632/oncotarget.v8i37 |
| [14] |
HERNANDEZ-GEA V, FRIEDMAN S L. Pathogenesis of liver fibrosis[J]. Annual Review of Pathology, 2011, 6:425-456.
doi: 10.1146/pathmechdis.2011.6.issue-1 |
| [15] |
MITTAL S, EL-SERAG H B, SADA Y H, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease[J]. Clinical Gastroenterology and Hepatology, 2016, 14(1):124-131.
doi: 10.1016/j.cgh.2015.07.019 pmid: 26196445 |
| [16] |
DYSON J, JAQUES B, CHATTOPADYHAY D, et al. Hepatocellular cancer:The impact of obesity, type 2 diabetes and a multidisciplinary team[J]. Journal of Hepatology, 2014, 60(1):110-117.
doi: 10.1016/j.jhep.2013.08.011 |
| [17] |
OGATA H, GOTO S, SATO K, et al. KEGG:Kyoto encyclopedia of genes and genomes[J]. Nucleic Acids Research, 1999, 27(1):29-34.
doi: 10.1093/nar/27.1.29 |
| [18] |
KANEHISA M. Toward understanding the origin and evolution of cellular organisms[J]. Protein Science, 2019, 28(11):1947-1951.
doi: 10.1002/pro.3715 pmid: 31441146 |
| [19] | KANEHISA M, FURUMICHI M, SATO Y, et al. KEGG:Integrating viruses and cellular organisms[J]. Nucleic Acids Research, 2021, 49(D1):545-551. |
| [20] |
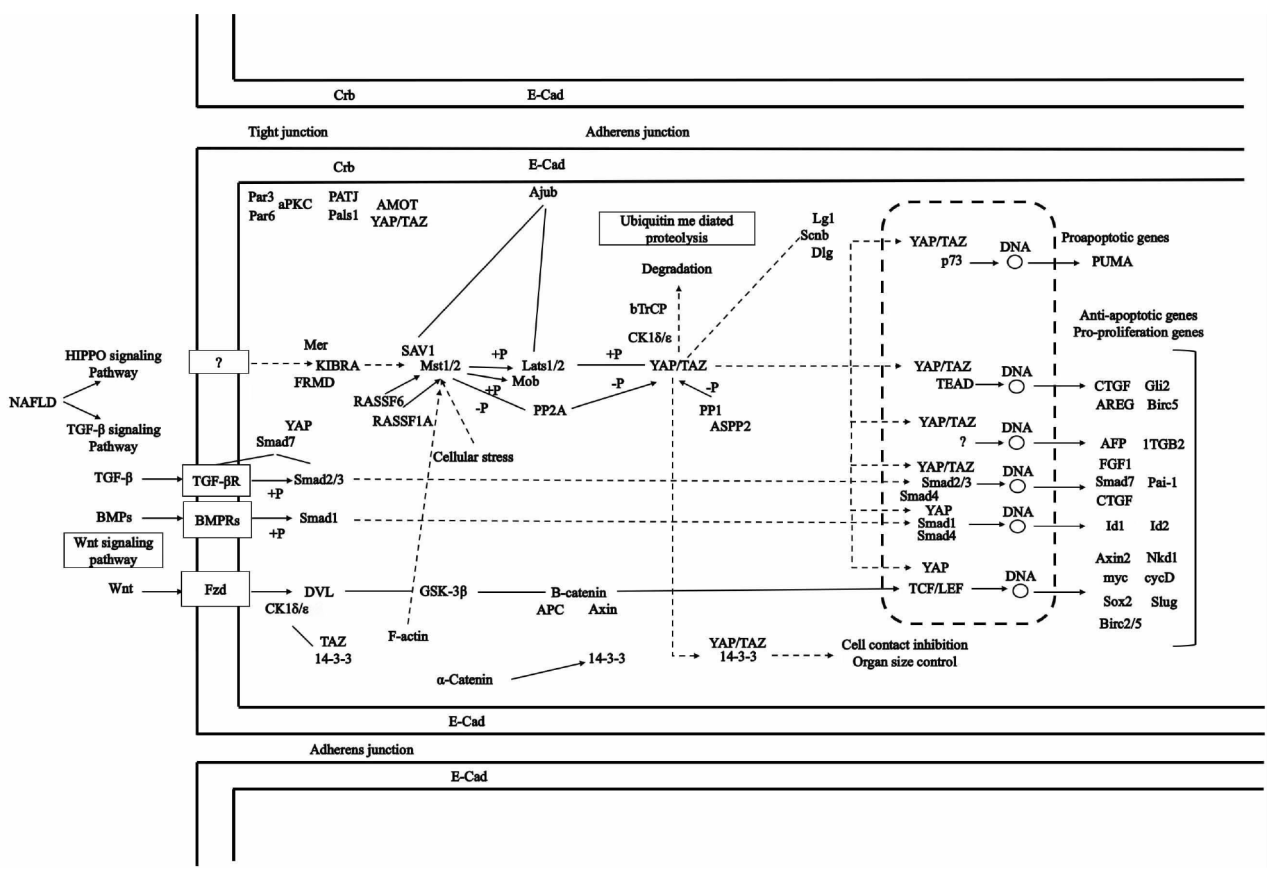
MENG Z P, MOROISHI T, GUAN K L. Mechanisms of Hippo pathway regulation[J]. Genes and Development, 2016, 30(1):1-17.
doi: 10.1101/gad.274027.115 |
| [21] |
MOROISHI T, HANSEN C G, GUAN K L. The emerging roles of YAP and TAZ in cancer[J]. Nature Reviews Cancer, 2015, 15(2):73-79.
doi: 10.1038/nrc3876 pmid: 25592648 |
| [22] |
MEDERACKE I, HSU C C, TROEGER J S, et al. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology[J]. Nature Communications, 2013, 4:2823.
doi: 10.1038/ncomms3823 pmid: 24264436 |
| [23] |
WANG X B, ZHENG Z, CAVIGLIA J M, et al. Hepatocyte TAZ/WWTR1 promotes inflammation and fibrosis in nonalcoholic steatohepatitis[J]. Cell Metabolism, 2016, 24(6):848-862.
doi: S1550-4131(16)30501-0 pmid: 28068223 |
| [24] |
YE J, LI T S, XU G, et al. JCAD promotes progression of nonalcoholic steatohepatitis to liver cancer by inhibiting LATS2 kinase activity[J]. Cancer Research, 2017, 77(19):5287-5300.
doi: 10.1158/0008-5472.CAN-17-0229 pmid: 28775168 |
| [25] |
AYLON Y, GERSHONI A, ROTKOPF R, et al. The LATS2 tumor suppressor inhibits SREBP and suppresses hepatic cholesterol accumulation[J]. Genes and Development, 2016, 30(7):786-797.
doi: 10.1101/gad.274167.115 |
| [26] |
CINGOLANI F, CZAJA M J. Regulation and functions of autophagic lipolysis[J]. Trends in Endocrinology and Metabolism, 2016, 27(10):696-705.
doi: S1043-2760(16)30064-9 pmid: 27365163 |
| [27] |
YU F X, ZHAO B, PANUPINTHU N, et al. Regulation of the hippo-YAP pathway by G-protein-coupled receptor signaling[J]. Cell, 2012, 150(4):780-791.
doi: 10.1016/j.cell.2012.06.037 |
| [28] |
TIAN Y, YANG B, QIU W N, et al. ER-residential Nogo-B accelerates NAFLD-associated HCC mediated by metabolic reprogramming of oxLDL lipophagy[J]. Nature Communications, 2019, 10:3391.
doi: 10.1038/s41467-019-11274-x pmid: 31358770 |
| [29] |
SONG M S, SALMENA L, PANDOLFI P P. The functions and regulation of the PTEN tumour suppressor[J]. Nature Reviews Molecular Cell Biology, 2012, 13(5):283-296.
doi: 10.1038/nrm3330 pmid: 22473468 |
| [30] |
KODAMA T, YI J, NEWBERG J Y, et al. Molecular profiling of nonalcoholic fatty liver disease-associated hepatocellular carcinoma using SB transposon mutagenesis[J]. Proceedings of the National Academy of Sciences of the United States of America, 2018, 115(44):10417-10426.
doi: 10.1073/pnas.1808968115 pmid: 30327349 |
| [31] |
JEONG S H, LIM D S. Insulin receptor substrate 2:A bridge between Hippo and AKT pathways[J]. BMB Reports, 2018, 51(5):209-210.
doi: 10.5483/BMBRep.2018.51.5.095 |
| [32] |
WANG Y H, VISCARRA J, KIM S J, et al. Transcriptional regulation of hepatic lipogenesis[J]. Nature Reviews Molecular Cell Biology, 2015, 16(11):678-689.
doi: 10.1038/nrm4074 pmid: 26490400 |
| [33] |
JEONG S H, KIM H B, KIM M C, et al. Hippo-mediated suppression of IRS2/AKT signaling prevents hepatic steatosis and liver cancer[J]. Journal of Clinical Investigation, 2018, 128(3):1010-1025.
doi: 10.1172/JCI95802 |
| [34] |
SHI G, LIAO P Y, CAI X L, et al. FoxO1 enhances differentiation and apoptosis in human primary keratinocytes[J]. Experimental Dermatology, 2018, 27(11):1254-1260.
doi: 10.1111/exd.13775 pmid: 30144329 |
| [35] |
MANNING B D, TOKER A. AKT/PKB signaling:Navigating the network[J]. Cell, 2017, 169(3):381-405.
doi: 10.1016/j.cell.2017.04.001 |
| [36] |
LIEN E C, DIBBLE C C, TOKER A. PI3K signaling in cancer:Beyond AKT[J]. Current Opinion in Cell Biology, 2017, 45:62-71.
doi: 10.1016/j.ceb.2017.02.007 |
| [37] |
WANG H J, LIU Y M, WANG D M, et al. The upstream pathway of mTOR-mediated autophagy in liver diseases[J]. Cells, 2019, 8(12):1597.
doi: 10.3390/cells8121597 |
| [38] |
HUANG T J, REN J J, ZHANG Q Q, et al. IGFBPrP1 accelerates autophagy and activation of hepatic stellate cells via mutual regulation between H19 and PI3K/AKT/mTOR pathway[J]. Biomedicine and Pharmacotherapy, 2019, 116:109034.
doi: 10.1016/j.biopha.2019.109034 |
| [39] |
NI H M, WILLIAMS J A, YANG H, et al. Targeting autophagy for the treatment of liver diseases[J]. Pharmacological Research, 2012, 66(6):463-474.
doi: 10.1016/j.phrs.2012.07.003 |
| [40] |
YE R F, DAI N G, HE Q K, et al. Comprehensive anti-tumor effect of Brusatol through inhibition of cell viability and promotion of apoptosis caused by autophagy via the PI3K/Akt/mTOR pathway in hepatocellular carcinoma[J]. Biomedicine and Pharmacotherapy, 2018, 105:962-973.
doi: S0753-3322(18)32020-1 pmid: 30021391 |
| [41] |
ZHANG M, CHI X M, QU N, et al. Long noncoding RNA lncARSR promotes hepatic lipogenesis via Akt/SREBP-1c pathway and contributes to the pathogenesis of nonalcoholic steatohepatitis[J]. Biochemical and Biophysical Research Communications, 2018, 499(1):66-70.
doi: S0006-291X(18)30619-3 pmid: 29555473 |
| [42] | MOLINA S A, MORIARTY H K, INFIELD D T, et al. Insulin signaling via the PI3-kinase/Akt pathway regulates airway glucose uptake and barrier function in a CFTR-dependent manner[J]. American Journal of Physiology Lung Cellular and Molecular Physiology, 2017, 312(5):688-702. |
| [43] |
COHEN P, ALESSI D R, CROSS D A E. PDK1, one of the missing links in insulin signal transduction?[J]. FEBS Letters, 1997, 410(1):3-10.
doi: 10.1016/s0014-5793(97)00490-0 pmid: 9247112 |
| [44] |
WINNAY J N, DIRICE E, LIEW C W, et al. p85α deficiency protects β-cells from endoplasmic reticulum stress-induced apoptosis[J]. Proceedings of the National Academy of Sciences of the United States of America, 2014, 111(3):1192-1197.
doi: 10.1073/pnas.1322564111 pmid: 24395790 |
| [45] |
NELSON V L B, JIANG Y P, DICKMAN K G, et al. Adipose tissue insulin resistance due to loss of PI3K p110α leads to decreased energy expenditure and obesity[J]. American Journal of Physiology-Endocrinology and Metabolism, 2014, 306(10):1205-1216.
doi: 10.1152/ajpendo.00625.2013 pmid: 24691033 |
| [46] |
BERETTA M, BAUER M, HIRSCH E. PI3K signaling in the pathogenesis of obesity:The cause and the cure[J]. Advances in Biological Regulation, 2015, 58:1-15.
doi: 10.1016/j.jbior.2014.11.004 |
| [47] |
ELLINGSGAARD H, HAUSELMANN I, SCHULER B, et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells[J]. Nature Medicine, 2011, 17(11):1481-1489.
doi: 10.1038/nm.2513 pmid: 22037645 |
| [48] |
LAGATHU C, YVAN-CHARVET L, BASTARD J, et al. Long-term treatment with interleukin-1β induces insulin resistance in murine and human adipocytes[J]. Diabetologia, 2006, 49(9):2162-2173.
doi: 10.1007/s00125-006-0335-z |
| [49] |
RONCERO I, ALVAREZ E, ACOSTA C, et al. Insulin-receptor substrate-2 (irs-2) is required for maintaining glucokinase and glucokinase regulatory protein expression in mouse liver[J]. PLoS ONE, 2013, 8(4):e58797.
doi: 10.1371/journal.pone.0058797 |
| [50] | YONEYAMA Y, LANZERSTORFER P, NIWA H, et al. IRS-1 acts as an endocytic regulator of IGF-Ⅰ receptor to facilitate sustained IGF signaling[J]. eLife, 2018, 7:32893. |
| [51] |
HATA A, CHEN Y G. TGF-β signaling from receptors to smads[J]. Cold Spring Harbor Perspectives in Biology, 2016, 8(9):a022061.
doi: 10.1101/cshperspect.a022061 |
| [52] |
MENG X M, NIKOLIC-PATERSON D J, LAN H Y. TGF-β:The master regulator of fibrosis[J]. Nature Reviews Nephrology, 2016, 12(6):325-338.
doi: 10.1038/nrneph.2016.48 |
| [53] |
ALKHOURI N, CARTER-KENT C, FELDSTEIN A E. Apoptosis in nonalcoholic fatty liver disease:Diagnostic and therapeutic implications[J]. Expert Review of Gastroenterology and Hepatology, 2011, 5(2):201-212.
doi: 10.1586/egh.11.6 |
| [54] |
BARREYRO F J, HOLOD S, FINOCCHIETTO P V, et al. The pan-caspase inhibitor Emricasan (IDN-6556) decreases liver injury and fibrosis in a murine model of non-alcoholic steatohepatitis[J]. Liver International, 2015, 35(3):953-966.
doi: 10.1111/liv.12570 pmid: 24750664 |
| [55] |
GUICCIARDI M E, GORES G J. Apoptosis as a mechanism for liver disease progression[J]. Seminars in Liver Disease, 2010, 30(4):402-410.
doi: 10.1055/s-0030-1267540 pmid: 20960379 |
| [56] |
LIU D C, WANG K, LI K, et al. Ets-1 deficiency alleviates nonalcoholic steatohepatitis via weakening TGF-β1 signaling-mediated hepatocyte apoptosis[J]. Cell Death and Disease, 2019, 10:458.
doi: 10.1038/s41419-019-1672-4 |
| [57] |
SUWA K, YAMAGUCHI T, YOSHIDA K, et al. Smad phospho-isoforms for hepatocellular carcinoma risk assessment in patients with nonalcoholic steatohepatitis[J]. Cancers, 2020, 12(2):286.
doi: 10.3390/cancers12020286 |
| [58] |
PEVERILL W, POWELL L W, SKOIEN R. Evolving concepts in the pathogenesis of NASH:Beyond steatosis and inflammation[J]. International Journal of Molecular Sciences, 2014, 15(5):8591-8638.
doi: 10.3390/ijms15058591 |
| [59] |
WANG Y, DU J H, NIU X M, et al. miR-130a-3p attenuates activation and induces apoptosis of hepatic stellate cells in nonalcoholic fibrosing steatohepatitis by directly targeting TGFBR1 and TGFBR2[J]. Cell Death and Disease, 2017, 8(5):e2792.
doi: 10.1038/cddis.2017.10 |
| [60] |
HUANG M H, KIM H G, ZHONG X L, et al. Sestrin 3 protects against diet-induced nonalcoholic steatohepatitis in mice through suppression of transforming growth factor β signal transduction[J]. Hepatology, 2020, 71(1):76-92.
doi: 10.1002/hep.30820 pmid: 31215672 |
| [61] |
TAKEGOSHI K, HONDA M, OKADA H, et al. Branched-chain amino acids prevent hepatic fibrosis and development of hepatocellular carcinoma in a non-alcoholic steatohepatitis mouse model[J]. Oncotarget, 2017, 8(11):18191-18205.
doi: 10.18632/oncotarget.15304 pmid: 28212548 |
| [62] | HART K M, FABRE T, SCIURBA J C, et al. Type 2 immunity is protective in metabolic disease but exacerbates NAFLD collaboratively with TGF-β[J]. Science Translational Medicine, 2017, 9(396):3694. |
| [63] |
ZHAO P, SALTIEL A R. From overnutrition to liver injury:AMP-activated protein kinase in nonalcoholic fatty liver diseases[J]. The Journal of Biological Chemistry, 2020, 295(34):12279-12289.
doi: 10.1074/jbc.REV120.011356 |
| [64] |
NOVIKOVA D S, GARABADZHIU A V, MELINO G, et al. AMP-activated protein kinase:Structure, function, and role in pathological processes[J]. Biochemistry (Moscow), 2015, 80(2):127-144.
doi: 10.1134/S0006297915020017 |
| [65] |
PARK K G, MIN A K, KOH E H, et al. Alpha-lipoic acid decreases hepatic lipogenesis through adenosine monophosphate-activated protein kinase (AMPK)-dependent and AMPK-independent pathways[J]. Hepatology, 2008, 48(5):1477-1486.
doi: 10.1002/hep.22496 |
| [66] |
SARAN U, HUMAR B, KOLLY P, et al. Hepatocellular carcinoma and lifestyles[J]. Journal of Hepatology, 2016, 64(1):203-214.
doi: 10.1016/j.jhep.2015.08.028 pmid: 26341826 |
| [67] |
GARCIA D, SHAW R J. AMPK:Mechanisms of cellular energy sensing and restoration of metabolic balance[J]. Molecular Cell, 2017, 66(6):789-800.
doi: 10.1016/j.molcel.2017.05.032 |
| [68] |
HARDIE D G, ROSS F A, HAWLEY S A. AMPK:A nutrient and energy sensor that maintains energy homeostasis[J]. Nature Reviews Molecular Cell Biology, 2012, 13(4):251-262.
doi: 10.1038/nrm3311 |
| [69] |
ZHAO P, SUN X L, CHAGGAN C, et al. An AMPK-caspase-6 axis controls liver damage in nonalcoholic steatohepatitis[J]. Science, 2020, 367(6478):652-660.
doi: 10.1126/science.aay0542 pmid: 32029622 |
| [70] |
BOUDABA N, MARION A, HUET C, et al. AMPK re-activation suppresses hepatic steatosis but its downregulation does not promote fatty liver development[J]. eBioMedicine, 2018, 28:194-209.
doi: S2352-3964(18)30008-2 pmid: 29343420 |
| [71] |
GARCIA D, HELLBERG K, CHAIX A, et al. Genetic liver-specific AMPK activation protects against diet-induced obesity and NAFLD[J]. Cell Reports, 2019, 26(1):192-208.
doi: S2211-1247(18)31966-1 pmid: 30605676 |
| [72] |
SAHA A K, JULIA X X, EBONY L, et al. Downregulation of AMPK accompanies leucine- and glucose-induced increases in protein synthesis and insulin resistance in rat skeletal muscle[J]. Diabetes, 2010, 59(10):2426-2434.
doi: 10.2337/db09-1870 pmid: 20682696 |
| [73] |
CHOTECHUANG N, AZZOUT-MARNICHE D, BOS C, et al. mTOR, AMPK, and GCN2 coordinate the adaptation of hepatic energy metabolic pathways in response to protein intake in the rat[J]. American Journal of Physiology-Endocrinology and Metabolism, 2009, 297(6):1313-1323.
doi: 10.1152/ajpendo.91000.2008 pmid: 19738034 |
| [74] |
DAVAL M, DIOT-DUPUY F, BAZIN R, et al. Anti-lipolytic action of AMP-activated protein kinase in rodent adipocytes[J]. Journal of Biological Chemistry, 2005, 280(26):25250-25257.
doi: 10.1074/jbc.M414222200 pmid: 15878856 |
| [75] |
JEON S M. Regulation and function of AMPK in physiology and diseases[J]. Experimental and Molecular Medicine, 2016, 48(7):e245.
doi: 10.1038/emm.2016.81 |
| [76] |
LI Y, XU S Q, MIHAYLOVA M M, et al. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice[J]. Cell Metabolism, 2011, 13(4):376-388.
doi: S1550-4131(11)00096-9 pmid: 21459323 |
| [77] |
HAN J B, WANG Y G. mTORC1 signaling in hepatic lipid metabolism[J]. Protein and Cell, 2018, 9(2):145-151.
doi: 10.1007/s13238-017-0409-3 |
| [78] |
SCHUSTER S, CABRERA D, ARRESE M, et al. Triggering and resolution of inflammation in NASH[J]. Nature Reviews Gastroenterology and Hepatology, 2018, 15(6):349-364.
doi: 10.1038/s41575-018-0009-6 |
| [79] |
HUANG B P, LIN C H, CHEN H M, et al. AMPK activation inhibits expression of proinflammatory mediators through downregulation of PI3K/p38 MAPK and NF-κB signaling in murine macrophages[J]. DNA and Cell Biology, 2015, 34(2):133-141.
doi: 10.1089/dna.2014.2630 |
| [80] |
O′NEILL L A J, HARDIE D G. Metabolism of inflammation limited by AMPK and pseudo-starvation[J]. Nature, 2013, 493(7432):346-355.
doi: 10.1038/nature11862 |
| [81] |
SALMINEN A, HYTTINEN J M T, KAARNIRANTA K. AMP-activated protein kinase inhibits NF-κB signaling and inflammation:Impact on healthspan and lifespan[J]. Journal of Molecular Medicine, 2011, 89(7):667-676.
doi: 10.1007/s00109-011-0748-0 |
| [82] |
ZHAO P, WONG K I, SUN X L, et al. TBK1 at the crossroads of inflammation and energy homeostasis in adipose tissue[J]. Cell, 2018, 172(4):731-743.
doi: S0092-8674(18)30042-4 pmid: 29425491 |
| [83] | XIONG Y, TORSONI A S, WU F H, et al. Hepatic NF-κB-inducing kinase (NIK) suppresses mouse liver regeneration in acute and chronic liver diseases[J]. eLife, 2018, 7:34152. |
| [84] |
ZHOU R B, TARDIVEL A, THORENS B, et al. Thioredoxin-interacting protein links oxidative stress to inflammasome activation[J]. Nature Immunology, 2010, 11(2):136-140.
doi: 10.1038/ni.1831 pmid: 20023662 |
| [85] |
DASGUPTA B, CHHIPA R R. Evolving lessons on the complex role of AMPK in normal physiology and cancer[J]. Trends in Pharmacological Sciences, 2016, 37(3):192-206.
doi: S0165-6147(15)00243-6 pmid: 26711141 |
| [86] |
CHENG J D, HUANG T L, LI Y F, et al. AMP-activated protein kinase suppresses the in vitro and in vivo proliferation of hepatocellular carcinoma[J]. PLoS ONE, 2014, 9(4):e93256.
doi: 10.1371/journal.pone.0093256 |
| [87] | LAWRENCE T. The nuclear factor NF-kappaB pathway in inflammation[J]. Cold Spring Harbor Perspectives in Biology, 2009, 1(6):a001651. |
| [88] |
ROLO A P, TEODORO J S, PALMEIRA C M. Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis[J]. Free Radical Biology and Medicine, 2012, 52(1):59-69.
doi: 10.1016/j.freeradbiomed.2011.10.003 pmid: 22064361 |
| [89] |
WANG X N, ZHANG R, SHE Z G, et al. Interferon regulatory factor 3 constrains IKKβ/NF-κB signaling to alleviate hepatic steatosis and insulin resistance[J]. Hepatology, 2014, 59(3):870-885.
doi: 10.1002/hep.v59.3 |
| [90] |
ARKAN M C, HEVENER A L, GRETEN F R, et al. IKK-beta links inflammation to obesity-induced insulin resistance[J]. Nature Medicine, 2005, 11(2):191-198.
doi: 10.1038/nm1185 pmid: 15685170 |
| [91] |
WANG P X, ZHANG X J, LUO P C, et al. Hepatocyte TRAF3 promotes liver steatosis and systemic insulin resistance through targeting TAK1-dependent signalling[J]. Nature Communications, 2016, 7:10592.
doi: 10.1038/ncomms10592 |
| [92] |
LUO W J, XU Q Y, WANG Q, et al. Effect of modulation of PPAR-γ activity on Kupffer cells M1/M2 polarization in the development of non-alcoholic fatty liver disease[J]. Scientific Reports, 2017, 7:44612.
doi: 10.1038/srep44612 pmid: 28300213 |
| [93] |
WANG X J, LI L, WANG H W, et al. Epoxyeicosatrienoic acids alleviate methionine-choline-deficient diet-induced non-alcoholic steatohepatitis in mice[J]. Scandinavian Journal of Immunology, 2019, 90(3):e12791.
doi: 10.1111/sji.2019.90.issue-3 |
| [94] |
UTZSCHNEIDER K M, KAHN S E. The role of insulin resistance in nonalcoholic fatty liver disease[J]. The Journal of Clinical Endocrinology and Metabolism, 2006, 91(12):4753-4761.
doi: 10.1210/jc.2006-0587 |
| [95] |
LI C X, GAO J G, WAN X Y, et al. Allyl isothiocyanate ameliorates lipid accumulation and inflammation in nonalcoholic fatty liver disease via the Sirt1/AMPK and NF-κB signaling pathways[J]. World Journal of Gastroenterology, 2019, 25(34):5120-5133.
doi: 10.3748/wjg.v25.i34.5120 |
| [96] |
ZHANG T P, HU J J, WANG X M, et al. microRNA-378 promotes hepatic inflammation and fibrosis via modulation of the NF-κB-TNFα pathway[J]. Journal of Hepatology, 2019, 70(1):87-96.
doi: S0168-8278(18)32376-6 pmid: 30218679 |
| [97] |
DONGIOVANNI P, DONATI B, FARES R, et al. PNPLA3 I148M polymorphism and progressive liver disease[J]. World Journal of Gastroenterology, 2013, 19(41):6969-6978.
doi: 10.3748/wjg.v19.i41.6969 pmid: 24222941 |
| [98] |
YUAN S H, LIU H X, YUAN D, et al. PNPLA3 I148M mediates the regulatory effect of NF-κB on inflammation in PA-treated HepG2 cells[J]. Journal of Cellular and Molecular Medicine, 2020, 24(2):1541-1552.
doi: 10.1111/jcmm.v24.2 |
| [1] | LU Ya′nan, DING Wenli, YUE Taojing, XU Bowen, HUANG Shucheng. Recent Progress in the Roles of Integrin in Regulating Bone Health in Livestock and Poultry via PI3K/Akt Signaling Pathway [J]. Animal Husbandry and Feed Science, 2024, 45(1): 120-128. |
| [2] | WEI Yuanyuan, Hongmei, WANG Haisheng. Transcriptome Sequencing Analysis Reveals the Possible Therapeutic Mechanisms of a Traditional Mongolian Medicine Honghua Qinggan 13 Flavor Pills in CCl4 Induced Intestinal Injury in Mice [J]. Animal Husbandry and Feed Science, 2023, 44(6): 13-21. |
| [3] | KONG Deqing, QIN Qing, ZHANG Chongyan, LIU Zhichen, XU Xiaolong, LAN Mingxi, WANG Yichuan, ZHANG Jingwen, ZHAO Dan, WANG Zhixin, LI Jinquan, LIU Zhihong. Research Progress in Different Exogenous Substances Affecting Muscle Fiber Development [J]. Animal Husbandry and Feed Science, 2023, 44(3): 55-62. |
| [4] | MAO Fei, CHENG Min, CHEN Xiaoliang, DUAN Ran, SUN Yang, LI Guojun, WANG Caiyun. Research Progress in Sperm Capacitation Associated Signaling Pathways and Detection Methods in Mammals [J]. Animal Husbandry and Feed Science, 2023, 44(3): 63-68. |
| [5] | LIN Ya-nan, ZHAO Yuan, SU Shao-feng, ZHAO Jun-li, LI Ya-jing, TAO Jin-shan, ZHANG Jian-qiang, WENG Ya-juan, WU Hui, WANG Xiu-mei, ZHAO Yi-ping. Characterization of mRNA Relative Expression Levels of NF-κB Signaling Pathway Associated Genes in Maternal and Fetal Gastrointestinal Tracts of Mongolian Horse [J]. Animal Husbandry and Feed Science, 2022, 43(5): 79-86. |
| [6] | CHEN Pan, XU Ting-ting, HE Yan-feng, LIU Kai-li, XIE Jing-fei, YUE Ke, ZHANG Chao-dong, LIN Lu-xi, CAO Qin-qin, HUANG Shu-cheng. Research Progress on Effects of Calcium and Phosphorus Metabolism on Animal Bone Health [J]. Animal Husbandry and Feed Science, 2022, 43(1): 39-45. |
| [7] | MA Chun-li, WANG Li, WANG Ling-hong, DONG Chao, PAN Hai-ting, BAO Yu-long. RNA-seq Analysis Reveals Novel Genes and Signaling Pathways Associated with APAP-induced Acute Liver Injury in Mice [J]. Animal Husbandry and Feed Science, 2021, 42(4): 1-6. |
| [8] | ZHANG Xin-zhuang, CAO Di, Gerelchimeg, Manglai. Research Advances on Molecular Regulatory Mechanisms of Oxidative Stress and Nutritional Strategies in Livestock and Poultry Production [J]. Animal Husbandry and Feed Science, 2021, 42(4): 29-36. |
| [9] | ZHANG Chao-dong, CAO Qin-qin, XU Ting-ting, LIN Lu-xi, YUE Ke, ZHENG Jing-jing, HUANG Shu-cheng. Effects of Total Flavonoids from Rhizoma Drynariae on Bone Metabolism and Action Mechanisms [J]. Animal Husbandry and Feed Science, 2021, 42(4): 118-123. |
| [10] | WU Hai-qing, MA Yue-jun, Wudubala, Gaowa, LI Yu-rong. Mining of Cashmere Yield Associated Genes in Alpas Cashmere Goats [J]. Animal Husbandry and Feed Science, 2020, 41(1): 34-41. |
| [11] | . Role of Nrf2-ARE Pathway in Oxidative Stress Injury and Its Relationship with Other Signaling Pathways [J]. Animal Husbandry and Feed Science, 2016, 37(3): 42-42. |
| [12] | . Estrogen Up-regulates β-defensin-2(SBD-2) Expression in Ovine Oviduct Epithelial Cells via GPR30 Signaling Pathway [J]. Animal Husbandry and Feed Science, 2016, 37(10): 4-4. |
| [13] | . Research Progress on Rspol Protein and Wnt Signaling Pathway and Their Roles in Sex Determination [J]. Animal Husbandry and Feed Science, 2015, 36(4): 50-50. |
| [14] | . Molecular Control of Liver and Pancreas Development [J]. Animal Husbandry and Feed Science, 2009, 30(6): 6-6. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||